Referrals have been and always will be a critical component of care delivery. Primary care physicians refer patients to specialists when they identify an issue that requires a more in depth analysis. As payers and providers shift to a value-based model, closing the loop on a referral is a critical issue that spans the care continuum.
Referrals without a 360X loop may lead to incomplete and often lower value care. Millions of referrals are made every year and far too many go uncompleted. Even with advancing technologies, many providers still rely on the traditional and outdated paper-based method. Handing out a name and a number, printing out a long list of organizations, or faxing a referral can be beneficial, but the process is inefficient, slow, and ineffective. When care is fragmented it may cause a delay in diagnosis and treatment, causing poor or worsened health outcomes.
Lack of referral tracking can lead to inefficiency and frustration. Up to 50% of referrals are not completed. Of the ones that are completed, notes are often not sent back to referring practices, leaving them unaware of new diagnoses or changes. Most practices lack established processes for closing the referral loop.
Denver Health, is a multi-specialty health care system that has served as Denver’s safety net health system for 150 years. It receives over 151,000 unique patient visits per year from a diverse community with complex health needs. Due to the extensive range of healthcare services offered by Denver Health, 95% of referrals are made to other Denver Health clinicians, all of whom share the same EHR.
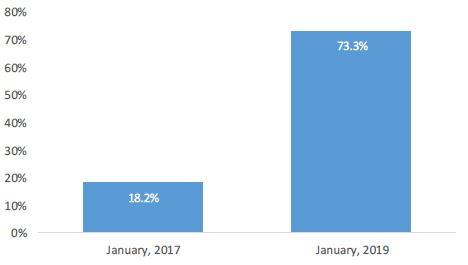
Denver Health identified two serious problems. First, patients often got lost in the scheduling process and never completed a referral visit. Second, even when referral visits were completed, referring clinicians were often unaware of the results and next steps, requiring the patient to serve as the communications go-between. A baseline measurement showed that post-consultation notes were sent to referring clinicians in only 18% of cases.
Once these problems were identified, a Denver Health quality team developed a close-the-loop process for referrals using the electronic capabilities of their own HER, shared with 95% of their network. Patients are pleased that they don’t fall through the cracks when referred to another clinic and happy that their doctors are communicating about their care. Measurable impact on Closing-the-Loop: In early 2017, Denver Health noted that the average rate of “closing-the-loop” for 43 specialty clinics was 18%, meaning that referral notes were sent back to the referring clinicians in only 18% of cases. Following implementation of the new processes, the average rate of referral notes rose from 18% to 73.3%.
Patient safety improved with the implementation of a full close-the-loop process; patients complete their referrals, and visit outcomes and plans of care are received by PCPs. In addition, patients are happy to have the health system support them with care coordination and trust the reliability of the process.
As a result of the close-the loop process, primary care clinicians started calling specialty clinicians to thank them for providing referral notes and care plans. As the success of the new seamless process became known, other patient touch points, such as the emergency department, dental clinics, and behavioral health, expressed interest in implementing close-the-loop measures as well.
At Medaflex, we wish that all practices would or could ‘Close the Loop’ as will be the case when interoperability becomes a universal reality. Until then, a patient PHI record to bridge the information gap may be one of the best tools available.

